As health, wellness, nutrition, and fitness coaches, one of the primary skills that you develop during your training is how to guide your clients toward adopting behaviors that make them healthier. You help them to achieve physical, mental, and social wellbeing.
The general population has the perception that access to information will naturally lead to behavior change.
Health professionals know change in health behaviors rarely takes place when someone simply knows which behaviors contribute to illness and which behaviors contribute to health.
If health behavior change were as simple as knowing what actions contribute to health, no one would smoke, drink alcohol, or eat ultra-processed foods, and most people on the planet would make exercise part of their daily activities.
Clearly, health behavior change is much more complex than simply having access to information.
Health behaviors result from a complex process of decisions, habits, mental state, social support, historical experiences with discrimination, access to healthcare, trauma, culture, economic access, and several others.
These dynamics of health behaviors are continually changing, and it can be ineffective to take action by trial and error with clients.
This article will provide you with an overview of health behavior science and cover some ineffective and effective methods of modifying health behaviors.
After reading this article, you will be equipped with the research-backed information and tools to help your clients make beneficial and long-lasting changes regarding their health.
What Are Health Behaviors?
Health behaviors are decisions and actions that shape health and wellbeing in individuals, as well as in populations.
Some experts refer to health behaviors as any action that influences health either by maintaining, promoting, or diminishing health status. In contrast, others see health behaviors only as those that positively impact health.
William Cockerham defines a health behavior, in the positive sense, as “the activity undertaken by individuals for the purpose of maintaining or enhancing their health, preventing health problems, or achieving a positive body image.”
Health behaviors aren’t necessarily limited to people who want to stay healthy, but also people who have a physical disability and people who have been diagnosed with chronic diseases and who wish to slow disease progression, manage the illness, or even contain or reverse the disease. They can achieve this through positive forms of health behavior, like a balanced diet, regular exercise, and avoiding smoking and drugs.
In the United States, the leading causes of illness and death are at least partially directly related to health behaviors, namely, poor diet, smoking, and high blood pressure.
The most critical health-related behaviors include:
- Diet
- Exercise, physical activity, and sedentarism
- Smoking
- Drugs
- Sex-related behaviors (like unprotected sex)
- Thoughts or actions that impact mental health
- Thoughts or actions that impact social health
As health and wellness professionals, as you read through this list, it might be clear to you in which of these behaviors you are best equipped to support your clients.

Why Do Your Clients Make the Choices They Do?
Health behaviors are the result of a complex interaction between social, environmental, and psychological influences. These are called “key determinants of health behaviors.”
Social Determinants of Health Behaviors
The social environment has a significant influence on how people make decisions for their health. These are crucial factors to consider as they make clear that health status is not merely the result of individual choice.
As the researcher Clare Xanthos and her team state, “explaining unhealthy behaviors simply as a matter of individual choice may be counterproductive since it leads toward a ‘blaming the victim approach’ whereby disadvantaged populations are blamed for using unhealthy coping mechanisms for dealing with their difficult social circumstances.”
In other words, social determinants of health can have a significant impact on health status since the social environment can encourage unhealthy behaviors and discourage healthy behaviors. For example, researchers have demonstrated that alcohol is disproportionally marketed toward Black communities.
That being said, there are several social determinants of health behaviors that are well-established. These include:
- Societal institutions
- Ideologies on a family, community, regional, national, and even global level
- Inequalities and discrimination, including racism and sexism
- Agency, or the power of an individual to make decisions and take actions
Environmental Determinants of Health Behaviors
The environment in which different individuals live, work, and those through which they move all have an influence on health behaviors. Some researchers refer to this as the “health ecosystem.” Through this model, the individual and their personal characteristics are influenced by working conditions, living conditions, social and environmental resources, and opportunities that are available in conjunction with the build and natural environment.
Access to parks and safe sidewalks; fresh, low-cost food; and stable, well-paying jobs with time for recreation all have an influence on how people make decisions for their health.
Environmental racism has an important role in the determinants of health behaviors. Environmental racism refers to the policies and actions carried out by public and private entities that explicitly put people of color at a disadvantage.
The study that coined the term “environmental racism” in 1987 demonstrated that hazardous waste facilities, which are known to be detrimental to health, were far more likely to be situated in Black and Latino communities than in areas populated by whites of the same socioeconomic class.
Other forms of environmental pollution, like the lack of access to clean water and living in cities with high levels of smog, also have a negative effect on health behavior.
Since all these factors aren’t only relevant to the individual but also to the health of entire populations under those same conditions, this is often the model of choice for public health professionals.
Psychological/Cognitive Determinants of Health Behaviors
The psychological and cognitive determinants of health behaviors refer to those that are centered on an individual’s knowledge or what he or she believes to be true in combination with a person’s confidence to make a change.
Other factors to consider regarding the psychological and cognitive determinants of health are mental health conditions, such as anxiety, depression, addictions, and eating disorders.
It is important to note that psychological trauma negatively impacts health risks later in life. Adverse child events (ACEs) are known to affect the health of adults later in life by inciting health-damaging lifestyle choices like overeating and smoking and because people who have been through adverse events tend to experience chronic stress, which is a risk factor for a range of diseases.
Since most fitness, health, and wellness professionals work with clients on an individual level, rather than on a community level, this is where they can make the most significant impact. For this reason, we will focus on health behavior change theory from a cognitive viewpoint, since it will likely be most useful for health and wellness coaches.
Some Considerations for Health Behaviors
Separate but related to health behavior science are the biological factors that influence health outcomes, like age, sex, and heredity factors.
Keep in mind that while there are some overarching reasons for certain behaviors, there are also specific reasons and motivators that are specific to each practice. In other words, we cannot always generalize that one factor is the reason behind all the actions a person takes that act for or against his or her health. For example, “low self-esteem” may influence your client’s motivation to exercise, but you cannot necessarily assume that low self-esteem is the reason for all negative health behaviors.
As health, fitness and wellness professionals, it isn’t necessary for you to identify the specific determinants of each of your clients’ health behaviors. However, understanding how different spheres of influence can have an impact on how your client makes choices can help you to identify diverse methods of introducing new health behaviors so that they meet your client’s needs.
Health Behavior Change Frameworks: An Overview
There are dozens of behavior change theories. Many of these theories are applied to, or even developed for, health-related behaviors.
Two popular behavior change theories are the Health Belief Model (HBM) and the Transtheoretical Model (TTM). The Health Belief Model is based on the idea that health behavior change is based on cognitive factors, or what people think about health problems and proposed solutions.
The Transtheoretical Model of behavior change, also known as the Stages of Change Model, is another widely used behavior change model that states that changing a behavior is not a coincidence but rather an active process. Different people are found in different stages of behavior change and readiness.
As a coach, you can refer to both the Health Belief Model and the Transtheoretical Model to gain a better understanding of your client’s attitudes and beliefs toward health behaviors and the concrete behaviors they carry out.
Below, we give you an overview of both models.
Transtheoretical Model
This model was developed by Prochaska and DiClemente with the goal of summarizing the unifying factors of several behavior change theories.
In this model, health behavior change is described as taking place over five stages: precontemplation, contemplation, preparation, action, and maintenance.
The strengths of the Transtheoretical Model include being able to locate a person’s progress toward a desired health behavior in a sequence, and it recognizes the possibility of and potential for relapse at any given stage.
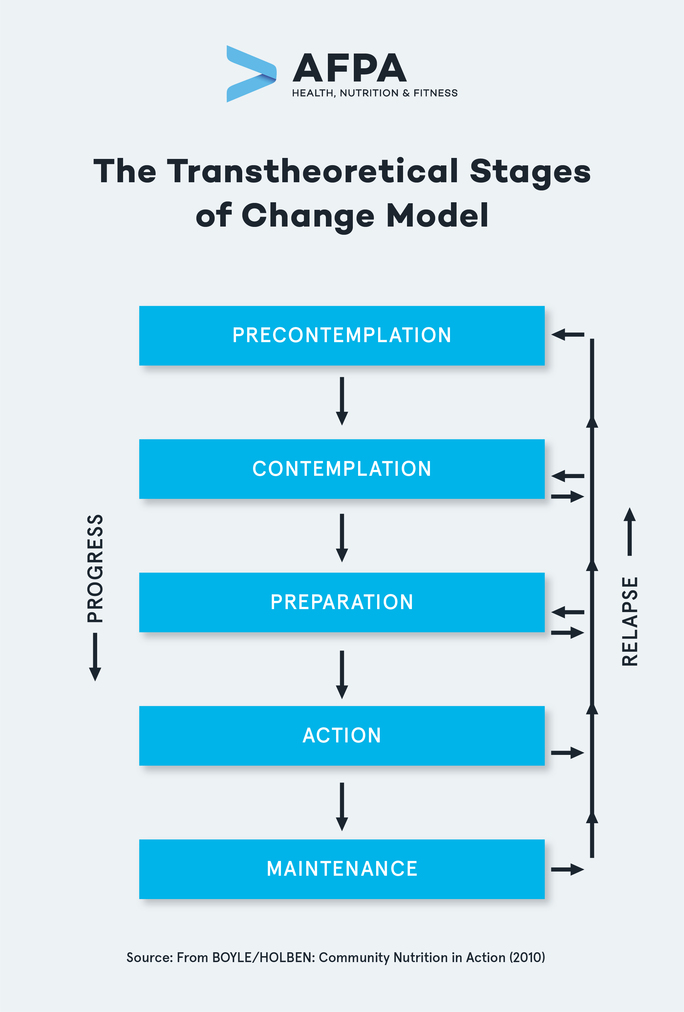
The stages of the Transtheoretical Model are:
- Precontemplation: A person at this stage doesn’t have an intention to change current behavior and may actively resist the efforts of others to change their behavior. This could be because they aren’t aware that there is a problem, don’t recognize their behavior as problematic for their health, or are facing feelings of hopelessness after having previously attempted to make a change.
- Contemplation: A person at the contemplation stage recognizes a need to change but has not yet taken action to make changes. They may see barriers to change that are perceived as bigger than the need to change. Some barriers may be economic limitations, inconvenience, a lack of support, or a lack of access to tools and resources seen as essential to make changes. Some of these barriers result from systemic social injustice.
- Preparation: A person at this stage is convinced that they need to make a change and they believe that the advantages of making a change in their health behavior outweigh the barriers or disadvantages. A person who is preparing to make change usually shows a willingness to try new things.
- Action: People in the action stage of behavior change have actively modified their behavior to adopt those that promote their health. The action stage can start as soon as one day after making the change to up to six months of consistently having adopted a new or modified behavior.
- Maintenance: A person who is in the maintenance stage of health behavior change has adopted the new or modified health-promoting behavior for more than six months. However, the person must actively work to maintain this behavior and avoid relapse.
Health Belief Model
The Health Belief Model is one of the oldest and most widely used health behavior change models, so there is more data to back it up and tools freely available. The HBM comes from the perspective of cognitive determinants behavior change for health, which is generally where most fitness, health, and wellness coaches have an influence.
Some of the psychological determinants of health behaviors, based on the Health Belief Model include:
- Perceived susceptibility, or the belief that a person has about their chances of getting sick or being affected by a condition. In other words, if a person feels that they aren’t at risk of getting lung cancer, then they might not be that averse to smoking.
- Perceived severity, or the belief about how serious different conditions are for an individual. For example, if a twenty-five-year-old person believes that the Coronavirus only affects older people, they might not be too worried about using a mask or keeping social distance.
- Perceived benefits, which is the belief that a person has about how taking an action will reduce the risk of getting ill or how much the activity will improve the current condition. If your client believes that following a plant-based diet will significantly reduce their high blood pressure, they are more likely to follow this type of diet.
- Perceived barriers, or the belief about the drawbacks of a particular action. If an action that may improve health is too expensive, not pleasant, or will take up too much time, these are all seen as barriers to making changes.
- Cues to action, or the events that occur that motivate someone to do something differently. If your client has a health scare, or if you provide information about behaviors that shock them to make a change, these are cues to action.
- Self-efficacy, or the confidence in a person’s ability to take action. If a person can visualize how different behaviors could result in improved health, and if they estimate they can realistically achieve those improvements, they are self-efficacious. Here, the health coach can have a crucial role in bringing out a sense of self-efficacy.
It is important to keep in mind that all behaviors and motivations are informed by trauma. Until the trauma is resolved, the pattern will perpetuate itself.
By completing the AFPA health coach certification program, you can develop the expertise and confidence needed to excel in your career as a health coach.
Here is a representation of how these factors come into play with each other:
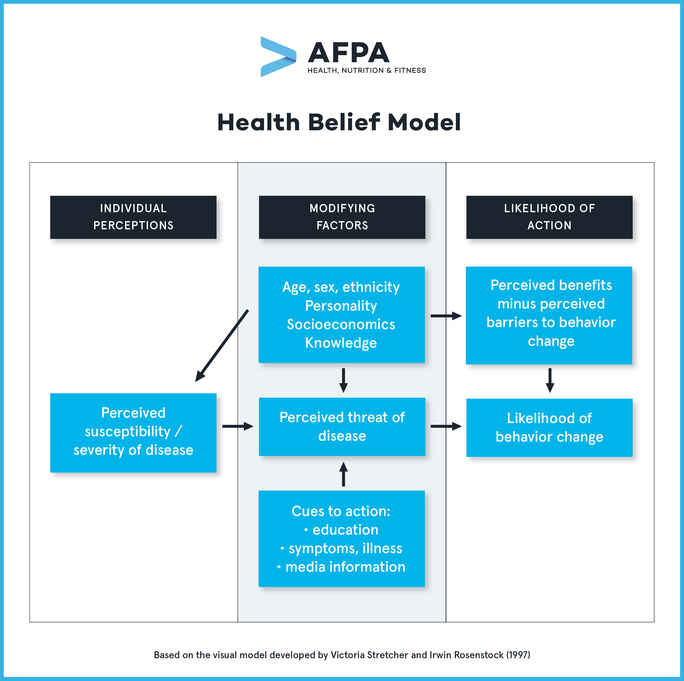
Factors that can modify the individual beliefs and resulting actions mentioned above include age, gender, ethnicity, personality, socioeconomics, and knowledge. You can refer to the section about the determinants of health behaviors for more information on the modifying factors of health beliefs.
Why We Are Where We Are: The Nutrition Transition
From a public health perspective, we are in a perplexing and seemingly contradictory time in history. Globally, most societies have greater access to a wide variety of goods year-round, but we have passed a point of achieving balanced nutrition, and instead, many communities are more likely to over-consume macronutrients while still being at risk for micronutrient deficiencies.
As opposed to the changes over several thousands of years of human development before now, these shifts in our health habits seem to act directly against the survival of the human race.
Public health experts describe changes in dietary patterns as nutrition transitions , and we are currently experiencing a significant one.
Nutrition transitions are phenomena where modernization, urbanization, economic development, and increased wealth lead to changes in diet. Researchers have identified five nutrition transition patterns across human history.
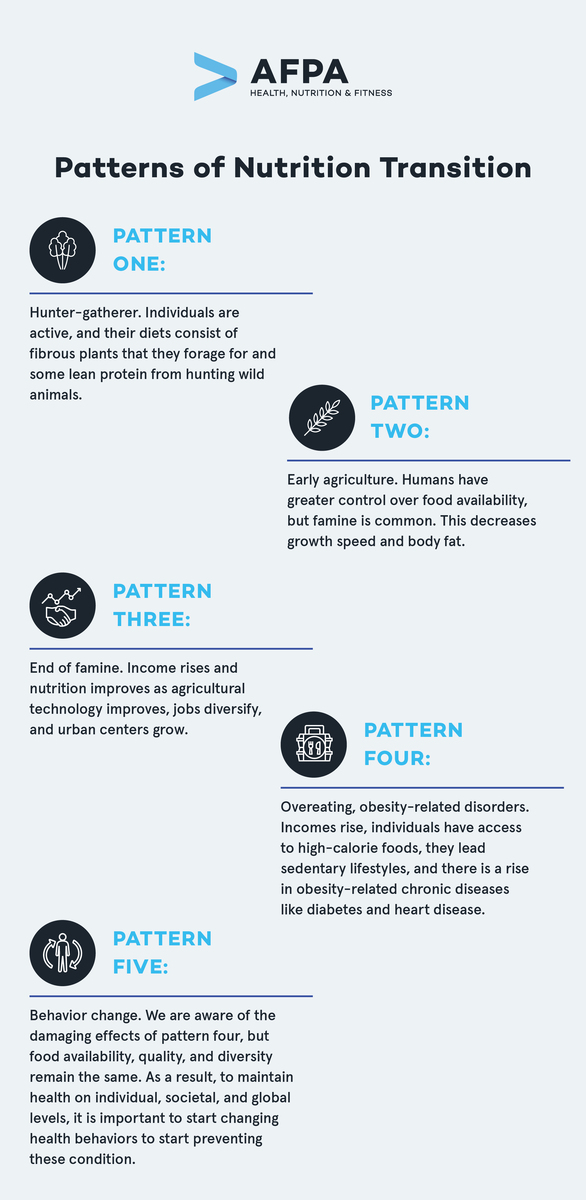
A Note About the Nutrition Transition from a Global Perspective
It is important to note, however, that while the nutrition transition, which is rooted in Western eating habits , is a global phenomenon, including in developing countries, there are regions in the world that have very different realities. These regions are still very vulnerable to famine and various forms of malnutrition, as was common in earlier patterns of nutrition transition.
For these reasons, as health and wellness professionals, it is essential to be aware that realities can be drastically different in different communities, and many of those realities may not be what we initially assume.
Why Is Knowledge About the Nutrition Transition Important for Health and Wellness Professionals?
At this moment in the history of human health, we are currently shifting from pattern four to pattern five. Different societies and individuals are moving at different paces.
As we transition into a pattern of health behaviors that require entire societies to start adopting behavior changes for their wellbeing, and even their survival, the role of health and wellness professionals becomes ever more critical.
From your experience as a health and wellness professional, you may be able to think of past clients or people you know that seem to embody pattern four (eating foods high in refined sugar, leading sedentary lifestyles, and developing metabolic disorders). In contrast, other clients may be fully ready to embrace pattern five, that of behavior change, where they are ready and committed to taking actions to prevent and treat disease.
You may also be able to think of individuals that are somewhere in between—they are aware of how their actions are negatively affecting their health. However, they are still adopting unhealthy behaviors because they are unsure about how to make the change, or they are worried about negative impacts on their mental health from making a change. This last scenario may resonate with you significantly—many people who look for the support of health and wellness coaches want to make a change, but they aren’t sure how to begin.
As health, wellness, fitness, and nutrition coaches explicitly trained to support and guide your clients toward health-promoting behavior changes, your role in fighting the obesity and obesity-related illness epidemic is becoming more and more essential to help move along the process with each of your clients.
Main Takeaways
A health and wellness coach has the goal of helping people adopt actions that improve their health status and overall wellbeing. Health and wellness professionals can more effectively help their clients make changes to unhealthy behaviors and motivate them to continue taking healthful action when they are informed about all of the factors that influence how they make decisions.
In this article, we also gave you an overview of other determinants of health behaviors that go beyond personal knowledge and choice so you can more sensitively approach the individual conditions in which your clients live and work, and how they may influence actions.
In later articles, we will provide you with the tools based on the Health Belief Model that can help you work with your clients to make effective and long-lasting change.




